If you feel worse in the second half of your cycle—more anxious, bloated, moody, or exhausted—you’re not alone. Many women automatically blame progesterone for these symptoms. But in most cases, it’s not progesterone itself—it’s the imbalance between oestrogen and progesterone that’s to blame.
This imbalance, often called oestrogen dominance, can occur even when your oestrogen levels appear “normal.” Contributing factors include chronic stress (which raises cortisol), cellular hypothyroidism, disrupted ovulation, inadequate nutrition, poor detoxification, and exposure to hormone-disrupting chemicals in the environment. Understanding the difference between oestrogen dominance and progesterone deficiency is key to restoring hormone balance—and feeling like yourself again.
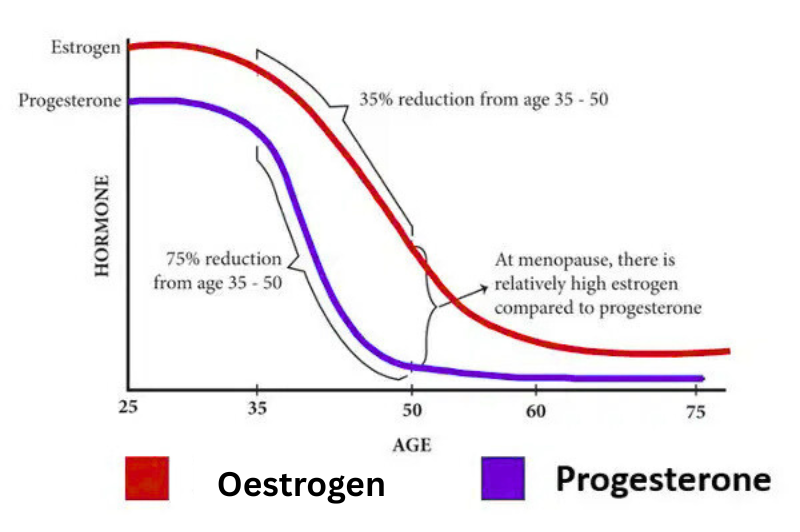
Progesterone: The First Hormone to Decline
Long before menopause, progesterone is typically the first hormone to drop. Why? Because it’s only produced when you ovulate—and ovulation often becomes less consistent as early as your mid-30s.
Even if your cycles seem regular, you might not be ovulating every time. Without ovulation, there’s no corpus luteum (the temporary gland that produces progesterone), which leaves oestrogen unopposed and can result in symptoms such as:
- Mood swings or anxiety
- Breast tenderness
- Hot flushes
- Heavy or irregular periods
- Bloating, water retention, and weight gain
- Poor sleep or waking around 3 a.m.
Conditions commonly associated with oestrogen dominance and/or progesterone deficiency include:
- Uterine fibroids
- Lumpy breasts or cysts
- Low libido
- PMS or PMDD
- Endometriosis
For women with PCOS, this imbalance may begin even earlier, as ovulation is often irregular or absent for long periods—leading to chronically low progesterone while oestrogen remains relatively high.
The Hidden Hormonal Burden of Modern Life
One major but often overlooked factor? Xenoestrogens—synthetic chemicals found in everyday products that mimic oestrogen in the body. These include:
| Plastics | (e.g., water bottles, containers, food wraps, seafood) |
| Personal care products | Cosmetics, perfumes, soaps, sanitation products & lotions |
| Cleaning products and household chemicals | laundry powders, fabric softeners, and dishwashing liquids, all fragrances |
| Pesticide, Herbicides, fungicides | on non-organic fruit and vegetables |
| Hormones | In non-organic meat, eggs and dairy |
| Industrial materials | like paint, carpets, and furniture |
| Air pollution | car exhaust, industrial fumes etc |
These compounds bind to oestrogen receptors and disrupt natural hormone signalling. Some increase oestrogenic activity; others desensitise receptors. Either way, they tip your system into imbalance—especially when progesterone is already declining.
Stress and Progesterone: A Complex Relationship
Let’s face it—who can honestly say they’re completely free from stress? For women, the pressure to appear as though we “have it all” is stronger than ever, often at the expense of our own well-being. Whether you’re building a career, raising a family, or navigating life solo, the mental load is real.

This chronic stress doesn’t just affect your mood—it directly impacts your hormonal balance.
When cortisol (your primary stress hormone) stays high, it can block progesterone receptors, making it harder for progesterone to function—even if you’re producing enough. This can lead to:
- Fatigue and burnout
- Anxiety or irritability
- Brain fog or difficulty concentrating
- Disrupted sleep
- Lowered immunity and increased inflammation
Even if you’re eating well, exercising, and taking supplements—if stress isn’t addressed, hormonal imbalances can persist.
Why Progesterone Still Matters—Even After Menopause
Many women are prescribed oestrogen-only hormone therapy or synthetic progestins—but these don’t mimic the effects of natural progesterone. (See our blog: “The Benefits of Personalised Menopause Hormone Replacement Therapy”)
What also matters is how you take progesterone.
Bioidentical progesterone, which matches your body’s natural structure, offers wide-ranging benefits:
| Calms the nervous system and improves sleep and mental health |
| Buffers the effects of stress and cortisol |
| Supports metabolism, thyroid, and brain function |
| Reduces inflammation and supports immune regulation |
| Balances estrogen’s growth-stimulating effects in breast and uterine tissues |
| Protects the heart, bones and skin |
After menopause, oestrogen production continues at low levels via fat cells and the adrenal glands. But progesterone production stops entirely, increasing the risk of functional oestrogen dominance—even into your 60s and 70s.

Forms of Progesterone: Oral, Topical, and Vaginal
Oral Progesterone
Oral micronised progesterone (e.g., Utrogestan) is often prescribed for its calming, sleep-supportive effects. However:
- It passes through the liver where it’s metabolised into other compounds.
- At higher doses (usually 200 mg and above), some metabolites may increase breast cancer risk, especially in sensitive individuals.
- Not all the hormone reaches circulation, and blood levels vary by person.
Topical (Transdermal) Progesterone
Absorbed through the skin via creams or gels
- Bypasses the liver—gentler on the system
- Lower risk of harmful metabolite formation.
- Provides more stable, adjustable dosing
Vaginal Progesterone
Delivered as suppositories or capsules, vaginal progesterone goes straight to the uterus and pelvic area:
- Highly effective for uterine protection.
- Often used in fertility treatments.
- Can have some systemic effects but may cause local irritation or inconvenience.
Does Topical Progesterone Have Systemic Effects?
Yes—when used properly, topical progesterone can have systemic effects. Clinical experience and research show that it:
- Relieves symptoms like anxiety, sleep issues, and hot flushes
- Is well tolerated by women sensitive to oral forms
- Offers steady support, though it may take longer to build therapeutic levels
As with all hormone therapy, personalisation is key—including the form, dose, and monitoring plan.
Hormone Balance Is a Two-Way Street
It’s not about demonising estrogen—or blindly replacing progesterone. It’s about restoring the right ratio between the two:
- Oestrogen prepares the body and encourages growth
- Progesterone counterbalances oestrogen’s growth-stimulating effects helps guide cells to develop in a more stable, mature way
- Both influence brain function, metabolism, immune response, and cycle regularity and much more.
Hormones follow the Goldilocks principle—they need to be ‘just right.’ Too much or too little of either can throw your body and mind out of balance.
What This Means for You
If you’re dealing with:
- PMS or irregular cycles
- Anxiety, mood swings, or poor sleep
- Weight gain or fatigue that doesn’t budge
- Brain fog or hormonal acne
… it might not be “just low oestrogen.” It could be:
- Progesterone loss from irregular or absent ovulation.
- Chronic stress interfering with progesterone’s action.
- Hidden Environmental xenoestrogens tipping your hormonal balance
By taking a systems-based approach, we help uncover the root cause—and design a plan that supports your hormones effectively.
At Preciva Health, We See the Full Picture
We don’t just treat symptoms—we uncover why they’re happening. Whether you’re navigating PCOS, perimenopause, or postmenopause, we assess:
- Your unique hormone patterns
- Stress load and lifestyle factors
- Environmental toxin exposure
- Nutritional and metabolic needs
Your hormones are powerful messengers. Your body is wise. Your symptoms are signals—asking for deeper support.
So you not only feel better now, but protect yourself for a better future.

You must be logged in to post a comment.