When it comes to hormone replacement therapy (HRT), the information available can be overwhelming—and often contradictory. Many women feel confused, uncertain, or worse, misinformed. The reality? Not all hormones are the same, and not every woman needs the same approach.
Why Hormone Therapy Must Be Personalised
Every woman enters perimenopause or menopause with a unique hormone profile. Visit my other post on Why a Comprehensive Integrative Approach, is Key to Managing Health during Perimenopause and Beyond.
Each woman has had her own unique health journey. This journey has been shaped by a wide range of personal factors, including:
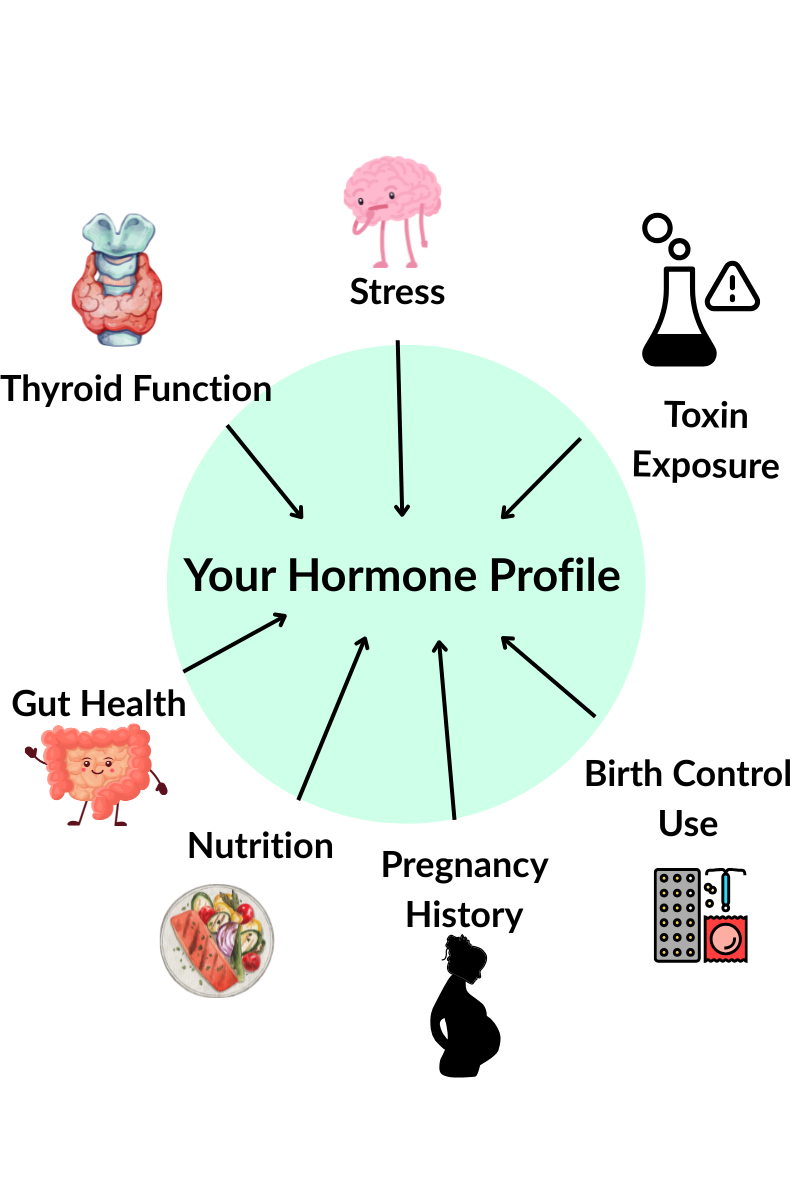
These variables influence how—and when—your estrogen, progesterone, and testosterone levels begin to shift. One woman may have a sharp decline in progesterone, while another may experience high estrogen and low testosterone. There is no universal hormonal pattern.
Because of this, a one-size-fits-all hormone therapy approach simply doesn’t work. In fact, giving a woman the wrong type or dose of hormone can do more harm than good.
A Look Back at HRT: The WHI Study and Synthetic Hormones
Many concerns about hormone therapy stem from the Women’s Health Initiative (WHI) study in the early 2000s. This research was halted early due to alarming health risks associated with the synthetic hormones used:
- 100% increase in Alzheimer’s risk
- 26% higher risk of invasive breast cancer
- 29% higher risk of heart attack
- 41% higher risk of stroke
- 200% increased risk of blood clots
But it’s important to note what hormones were studied. The WHI used:
Premarin: a mix of estrogens derived from the urine of pregnant horses. It contains compounds not found in the human body. These are up to 1,000 times more potent than human estrogen. This leads to overstimulation and less of the desired beneficial effects of natural estrogen made by the body.
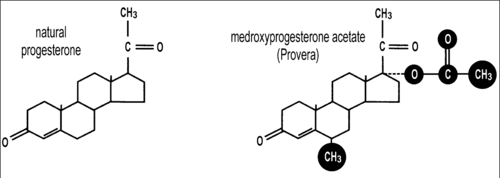
Provera, is a brand name for a Medroxyprogesterone acetate (MPA), a synthetic progestin found in the contraceptive implant Depo-provera. Most hormonal contraceptives contain different synthetic versions of either a combination of estrogen and progestin or progestin alone. All progestins are structurally different from the body’s natural progesterone. Any change in structure of a hormones changes its actions.
Let’s be clear: Bioidentical hormones were not used in the WHI study.

Bioidentical vs. Body-Identical vs. Synthetic Hormones
What Are Bioidentical Hormones?
Bioidentical hormones are chemically identical to those your body naturally produces. They are:
- Derived from plant-based sources. These often include yam or soy sterols. They share the same structure as cholesterol, from which sex hormones are derived.
- Custom-compounded by specialised pharmacies
- Tailored in dose and form to fit each individual
They match your body’s natural hormones. This allows them to be more easily recognised, metabolised, and excreted. This match makes them a safer, more compatible option when used correctly.
What are Body-identical Hormones?
These hormones are also structurally identical to human hormones but are produced by pharmaceutical companies in standardised doses. They are often prescribed without personalisation, and the fixed doses may be too high—or too low—for many women. Over time, this can lead to unwanted side effects or long-term health risks.
This is particularly true, if the management plan does not account for individual differences in hormone processing. Once inside the body, it can lead to serious consequences which may not be apparent right away.
What About Synthetic Hormones?
Synthetic hormones, like those used in the WHI study, are structurally different from natural human hormones. Most forms of hormonal contraceptives fall into this category. These chemical modifications make them patentable for pharmaceutical companies—but less compatible with the body, potentially leading to harmful effects.
The Power of Bioidentical Hormones
When prescribed and monitored correctly, bioidentical hormones offer powerful benefits without the risks associated with synthetic drugs. That’s because your body already knows how to interact with them.
When prescribed with care and precision, bioidentical hormones can offer powerful benefits:
- Relieve hot flashes, night sweats, insomnia, and mood changes
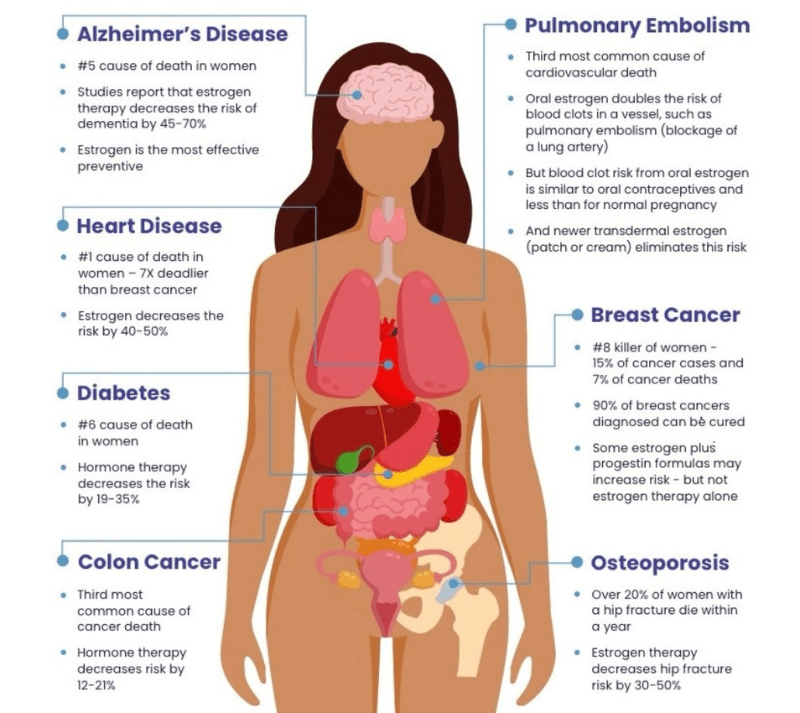
- Protect your heart, reducing heart attack risk by up to 50%
- Improve bone density and prevent osteoporosis
- Enhance brain function, memory, and mood
- Support a healthy immune system and metabolism.
Even estriol, the weakest of the three estrogens, offers unique benefits. In addition to its support in vaginal and urinary health, it also has anti-cancer properties. See my post on The Case for a Personalised, Integrative Approach to HRT: Moving Beyond Myths and Misconceptions
But hormones are powerful messengers. Too much of a good thing can still be as harmful, as not having enough protection. They must be dosed appropriately and in correct balance with other hormones. This is why ongoing testing, expert guidance from skilled practitioners trained in bioidentical hormone therapy, and tailored dosing are essential.
Why Isn’t This the Standard?
Unfortunately, bioidentical hormone therapy is not commonly taught in conventional medical training. Additionally, true bioidentical hormones can’t be patented. Therefore, they don’t attract the same research funding or pharmaceutical marketing as synthetic drugs.
Doctors who offer this approach must undergo additional, specialised training in functional and integrative medicine.
Do Bioidentical Hormones Increase Cancer Risk?
Not when used intelligently and in balance.
A 2008 study involved over 80,000 women. It showed no increased risk of breast cancer in those using bioidentical estrogen and progesterone. In fact, balanced hormone therapy—especially when paired with good lifestyle habits—may be protective.
Testosterone, often overlooked in women, is another important player. It’s used in some breast cancer treatments due to its tissue-regulating effects. It also supports bone, heart, brain, and sexual health in women.
The Bottom Line: Hormones Are Just One Piece of the Puzzle
Hormone therapy should never stand alone. Personalised bioidentical hormone therapy is just one part of a holistic strategy. A true path to hormone balance should support:
- Gut health (critical for hormone metabolism and elimination)
- Liver detox pathways
- Adrenal and thyroid function
- Nutritional balance and lifestyle
- Stress and sleep
This approach best supports your body through its natural transitions, helping to restore balance and vitality.
Should You Take Bioidentical Hormones?
That’s a decision best made in partnership with a qualified practitioner. Menopause is a natural life stage, not a disease. Your symptoms should be addressed if they are impacting your quality of life. Alternatively, you might want to take a proactive approach to long-term wellness.
When done properly, bioidentical hormone therapy can help restore energy, clarity, emotional balance, and vitality. But beyond symptom relief, there are significant long-term benefits. Optimally balanced hormones may help reduce the risk of chronic diseases. These include osteoporosis, cardiovascular disease, cognitive decline, metabolic syndrome and cancer.
This makes personalised hormone therapy not just a comfort-based decision—but potentially a powerful tool for preventive health.
Final Thoughts
Bioidentical hormones aren’t magic. But in the right hands, and with a personalised plan, they can help you feel like you again.
If you’re considering hormone therapy, don’t settle for standard protocols or rushed prescriptions. Your body is unique. Your hormones should be too.
Ready for a Truly Personalised Approach?
Dr. Rahna at Preciva Health specialises in customised bioidentical hormone therapy, designed to match your unique hormone profile and health history. Whether you’re in early perimenopause or navigating full menopause, she provides expert care that moves beyond a one-size-fits-all model.


Comments
3 responses to “The Benefits of Personalised Menopause Hormone Replacement Therapy”
[…] BOOK A CONSULTATION The Case for a Personalised, Integrative Approach to HRT: Moving Beyond Myths and Misconceptions The Benefits of Personalised Hormone Replacement Therapy […]
[…] Why a Comprehensive Integrative Approach, is Key to Managing Health during Perimenopause and Beyond. The Benefits of Personalised Hormone Replacement Therapy […]
[…] Many women are prescribed oestrogen-only hormone therapy or synthetic progestins—but these don’t mimic the effects of natural progesterone. (See our blog: “The Benefits of Personalised Menopause Hormone Replacement Therapy”) […]